Home »
Our Services » Oral Prophylaxis
Oral Prophylaxis
 |
Important
Periodontal Definitions
- Calculus: Only flossing and brushing are sometimes are unable to completely eradicate plaque bacteria. The accumulation of mineralized plaque that forms on the root of the tooth and/or on the crown. Calculus is also known as tartar.
- Gingiva: The soft tissue that surrounds the jawbone. Gingiva is also called as gums.
 |
- Gingivectomy: The surgical procedure to reshape or repair the gingiva.
- Gingivitis: Gum tissue/Gingival infection or inflammation. Gingivitis is the early phase of periodontal disease.
- Gingivoplasty: A surgical method to reshape/repair gingival.
- Graft: A portion of gingival tissue or artificial material aligned in contact with tissue to restore a shortcoming or aid a deficiency.
- Gum: See gingiva.
- Periodontal: 'Peri' means around and 'odont' means tooth hence, periodontal means any issue connected to the bone or tissue that supplements a tooth.
- Periodontal disease: Condition in which ligaments, gingiva, neighbouring tissue or bone supporting the tooth gets infected or inflamed. Periodontal disease can be classified into two main types viz. Gingivitis and Periodontitis. Periodontal disease can also be referred to as Pyorrhea or Gum disease.
- Periodontal pocket: An irregular increase in depth of the gum rift. Destruction of ligament that connects tooth to the gum and bone lying beneath it due to infection or disease forms a periodontal pocket.
- Periodontal surgery: Gum and jawbone treatment by means of surgical method is called as periodontal surgery.
- Periodontics: The special stream of dentistry that handles and treats bone that supports the teeth and gingival tissue.
- Periodontist: An expert with special training in surgical treatment of periodontal diseases.
- Periodontitis: Periodontal ligament, jawbone, gingival, bone or supplementary structure inflammation is known as Periodontitis.
|
- Plaque: Accumulation of bacteria, saliva and food particles that produce a thin sticky film both below and above the gum is called as plaque. Ignorance leads to serious problems of gingiva and tooth.
- Tartar: Refer Calculus definition.
What exactly is a periodontal disease?
Periodontal disease, also known as gingival
disease, pyorrhea or Periodontitis, is a complicated disease which can
be chronic or acute with non-active phase and flare ups, like other
chronic diseases. Inflammation of the gum tissue and the subsequent
damage to the bone that binds the teeth in the jaw by the inflammatory
process is known as periodontal disease. In grown ups, Periodontal
disease is the leading cause of tooth loss. The risk of contracting
other health issues increases during a periodontal disease.
What are the factors that lead to a periodontal
disease?
In its most fundamental state, the reply to
this question is bacteria. A human's oral cavity houses about 450
varieties of bacteria out of which a few cause periodontal diseases. The
damage done to the human can be attributed equally to direct destruction
caused by the toxins release by the bacteria and immune system
inflammation.
Which factors contribute to periodontal disease?
According to the latest studies, following
factors contribute to a periodontal disease; medications taken by
patients, type(s) of bacteria existing, general health and immune system
condition, tobacco products, alcohol, tooth alignment, saliva
(Viscosity, pH, amount) and finally, poor oral hygiene routine.
Significance of gum tissue
Human teeth maintain their position because of
the gingival tissue that is present on top of the bone. The part of the
gum can be seen is about 2-3 mm higher than the true attachment of the
gingiva to the tooth in health that creates a portion that appears like
a turtleneck collar. This particular space is the most common area of
bacterial housing and growth. A localized infection is caused by the
harmful toxins released by the bacteria residing in the space. This
inflammation caused by the bacteria damages the fibres that connect the
tooth and the gingiva. Periodontal disease's typical progressive nature
can be seen if the inflammation is allowed to penetrate to deeper layers
of the bone and gingiva.
What do you mean by Gingivitis?
 |
The state of the gingiva in which gums become
red and bleed while brushing, chewing or flossing due to inflammation of
gums is called as Gingivitis. The harbinger of a periodontal disease is
the inflammation of gingiva that must take place before the bone is
damaged. Sometimes, a large amount of time passes between inflammation
of gingiva and and destruction of the bone due to penetration of
inflammatory process. Mere observation is not enough to realize the
difference between periodontal disease and gingivitis. A periodontal
examination is must to diagnose a periodontal disease.
What happens during a periodontal examination?
 |
There are various stages of a periodontal
examination which are as follows:
- Periodontal probing in which the depth of the crevice around each tooth is measured and visual observation of gingiva and teeth is done.
- Supplementary bone evaluation by taking X-rays.
- Dental history and general health evaluation and review.
- Tooth alignment and 'bite' evaluation.
- Plaque is microscopically examined.
- Added diagnostic tools as designated.
What are the symptoms/signs of a periodontal
disease?
A periodontal examination only can be used to
actually diagnose a periodontal disease even though various symptoms and
signs can be seen in patients suffering from it. Areas of the bone
damaged by a periodontal disease cannot always be determined by taking
X-rays. We've still compiled a list of tell-tale signs as follows:
- Gingival bleeding while brushing.
- Swelling of gums or tenderness in gingival tissue.
- Increase in gap between teeth and gingiva.
- Formation of pus in the gap between teeth and gingiva.
- Misaligned and loose permanent teeth.
- Change in bite.
- Partial denture fitting problems.
- Peculiar taste or bad breath also known as halitosis.
Do any types of periodontal disease exist?
 |
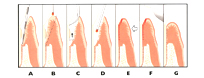
Adult Periodontitis is the most predominant
form of periodontal diseases. Depending on the level of bone loss, it
can be categorized into severe, moderate or mild. The state in which the
periodontal probe depth measures between 4-5 mm is known as mild
periodontal disease. The state in which the periodontal probe depth
measures between 6-7 mm is known as moderate periodontal disease. In
cases in which the periodontal probe depth is more than 8 mm is known as
severe periodontal disease. The risk of tooth loss increases with
increase in measurement of periodontal probe depth. Human tooth are
about 10-12 mm in length. A difference is found in measurements in
different regions surrounding the tooth.
Is periodontal disease infectious?
Periodontal disease is infectious. More
information can be found in the microscopic examination of plaque
section
How can a periodontal disease be treated?
Depending on the severity of the periodontal
disease, different types of treatments are available.
Reestablishment of healthy gingiva and their preservation to shield the oral cavity against future infections is the common denominator of all types of treatments of periodontal disease. Long lasting success can be achieved only through regular and effective eradication of bacteria.
Root planing or deep scaling is the primary form of treatment. It is the most conventional treatment accessible and is normally referred to as the Non-Surgical approach. This is more or less performed with local anesthesia and hardly causes side effects. First treatment is not enough to remove all the debris and deposits situated at a deeper level in the periodontal pockets and hence, each pocket is treated multiple times to ensure complete eradication of all harmful things. The process of the disease is eliminated and the gingiva reattaches itself a bit higher than earlier which makes it a better shield against future diseases. There are multiple options to improve these results which includes homecare techniques too. Advanced therapy which is called as Periostat which involves using a Collagenase inhibitor, and antibiotics are the other forms of treatment.
Performing periodontal surgery is the second leading alternative of treatment. Surgery does not provide a cure for the disease. A more manageable condition is created using surgery. A Gingivectomy is the simplest type of periodontal surgery. It involves removal of infected gingival tissue through surgical methods along with lower level healing of the gingiva. Level of tissue loss depends on the depth of the periodontal pocket. "Flap" procedures are the most common ones. While there are various types of "flaps" and various techniques, the aim is to temporarily shift the gum back while the surgery is being performed, eradicate the underlying disease and if required, alter the bone contour. The gingival tissue is realigned using sutures. Original position of the gingiva is never achieved after the surgery though the gingiva does reattach itself at a level higher than earlier. Using artificial bone matrix that encourages bone growth and implantation of new bone are the other types of surgical methods. Tooth removal or tooth extraction is the last type of treatment. Undoubtedly, the aim of any treatment is to preserve the teeth, nevertheless there are situations when the bone damage is so high around one or more teeth that it endangers the tooth adjacent to it. If the neighbouring tooth has amount of bone that can effectively be treated by one of the techniques mentioned above, yet the adjacent tooth cannot, then extraction of the unpromising tooth can only aid in the long term prognosis.
It is not unusual to discover periodontally involved teeth frequently respond optimistically to root canal treatment. A lot of studies have discovered periodontal disease causing bacteria inside the tooth. Elimination of such bacteria is not possible through the use of antibiotics.
Several upper molars, which typically possess three roots, frequently respond optimistically to the extraction of one of the lesser roots which is known as root amputation.
'Bite' and tooth alignment are vital factors. An aggravation of the underlying periodontal disease happens when more pressure is exerted on the teeth and the supplementary bone than it can bear. The decisive triumphant treatment of periodontal disease typically involves some type of orthodontic treatment and/or 'bite' adjustment.
A remission of disease occurs in case a regular and thorough removal of bacteria does not take place even though the there is a reestablishment of healthy gingival condition through treatment.
Reestablishment of healthy gingiva and their preservation to shield the oral cavity against future infections is the common denominator of all types of treatments of periodontal disease. Long lasting success can be achieved only through regular and effective eradication of bacteria.
Root planing or deep scaling is the primary form of treatment. It is the most conventional treatment accessible and is normally referred to as the Non-Surgical approach. This is more or less performed with local anesthesia and hardly causes side effects. First treatment is not enough to remove all the debris and deposits situated at a deeper level in the periodontal pockets and hence, each pocket is treated multiple times to ensure complete eradication of all harmful things. The process of the disease is eliminated and the gingiva reattaches itself a bit higher than earlier which makes it a better shield against future diseases. There are multiple options to improve these results which includes homecare techniques too. Advanced therapy which is called as Periostat which involves using a Collagenase inhibitor, and antibiotics are the other forms of treatment.
Performing periodontal surgery is the second leading alternative of treatment. Surgery does not provide a cure for the disease. A more manageable condition is created using surgery. A Gingivectomy is the simplest type of periodontal surgery. It involves removal of infected gingival tissue through surgical methods along with lower level healing of the gingiva. Level of tissue loss depends on the depth of the periodontal pocket. "Flap" procedures are the most common ones. While there are various types of "flaps" and various techniques, the aim is to temporarily shift the gum back while the surgery is being performed, eradicate the underlying disease and if required, alter the bone contour. The gingival tissue is realigned using sutures. Original position of the gingiva is never achieved after the surgery though the gingiva does reattach itself at a level higher than earlier. Using artificial bone matrix that encourages bone growth and implantation of new bone are the other types of surgical methods. Tooth removal or tooth extraction is the last type of treatment. Undoubtedly, the aim of any treatment is to preserve the teeth, nevertheless there are situations when the bone damage is so high around one or more teeth that it endangers the tooth adjacent to it. If the neighbouring tooth has amount of bone that can effectively be treated by one of the techniques mentioned above, yet the adjacent tooth cannot, then extraction of the unpromising tooth can only aid in the long term prognosis.
It is not unusual to discover periodontally involved teeth frequently respond optimistically to root canal treatment. A lot of studies have discovered periodontal disease causing bacteria inside the tooth. Elimination of such bacteria is not possible through the use of antibiotics.
Several upper molars, which typically possess three roots, frequently respond optimistically to the extraction of one of the lesser roots which is known as root amputation.
'Bite' and tooth alignment are vital factors. An aggravation of the underlying periodontal disease happens when more pressure is exerted on the teeth and the supplementary bone than it can bear. The decisive triumphant treatment of periodontal disease typically involves some type of orthodontic treatment and/or 'bite' adjustment.
A remission of disease occurs in case a regular and thorough removal of bacteria does not take place even though the there is a reestablishment of healthy gingival condition through treatment.
What do you mean by Gum Recession?
The shrinking away of gingiva from the chewing
surface or biting edge of the tooth due to destruction of gingiva and
supplementary bone is referred to as Gum Recession. The expression
''long in the tooth'' can be attributed to this condition. Both
periodontal disease and excessive exertion of pressure on the teeth can
lead to gum recession. Brushing does not lead to gum recession at all.
Progressive destruction of the attachment of the gingiva till the root
due to inflammation caused by periodontal disease leads to gum
recession.
How to treat Gum Recession?
The management depends on the cause and nature
of the problem . Early treatment can merely be desensitization of the
root contour in case of occurrence of tooth surface sensitivity. In some
cases a bonded filling can function as a shield against temperature.
Noticeable conditions of gum recession can be treated by using the most
common treatment called as gingival tissue grafting. We recommend using
an orthodontic brace and/or bite adjustment in case improper 'bite' is
the dominant factor.